
Trigeminal Neuralgia Trigger Checker
How This Tool Works
Based on clinical research, certain activities and stimuli trigger trigeminal neuralgia attacks. Select the activities you encounter daily to estimate your risk level. This tool doesn't diagnose but helps identify patterns to discuss with your doctor.
Daily Activities & Triggers
Your Trigger Assessment
When people talk about pain, they often think of broken bones or burns. But some of the worst pain you can feel doesn’t come from an injury you can see-it comes from a damaged nerve. And among all the nerves in the human body, one stands out as the most excruciating: the trigeminal nerve.
Why the trigeminal nerve hurts so badly
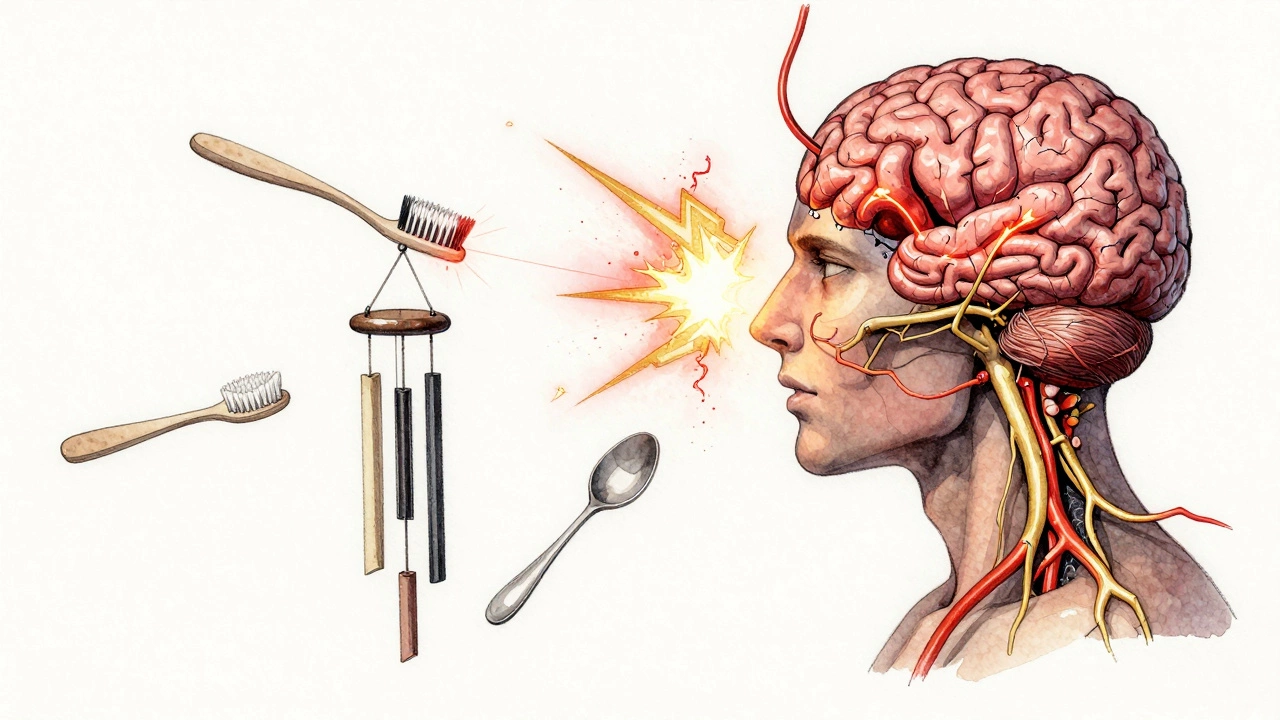
The trigeminal nerve is the fifth cranial nerve, and it’s responsible for sensation in your face. It branches out from your brainstem to your forehead, cheeks, and jaw. You use it every time you feel a breeze on your skin, bite into an apple, or brush your teeth. When it gets damaged, it doesn’t just send pain signals-it sends them like a faulty wire sparking nonstop.
This condition is called trigeminal neuralgia. It’s not common, affecting about 1 in 10,000 people each year. But for those who have it, the pain is unlike anything else. It strikes like an electric shock-sudden, sharp, and lasting only a second or two. But those seconds repeat. Dozens of times a day. Sometimes hundreds.
Patients describe it as being stabbed with a hot knife, or like someone is drilling into their cheek. One woman from Christchurch told her doctor she’d rather have a tooth pulled without anesthesia than endure another episode. That’s how bad it gets.
What triggers the pain
What makes trigeminal neuralgia even more cruel is how little it takes to set it off. A light touch. A gust of wind. Chewing. Talking. Even smiling. Many people avoid brushing their teeth, washing their face, or going outside because the risk of pain is too high. Some stop eating solid food because chewing triggers attacks. Others stop talking altogether to avoid the next wave of agony.
The most common cause is a blood vessel pressing against the nerve at the base of the skull. Over time, the constant pressure wears away the nerve’s protective coating, like fraying insulation on a wire. That’s when the nerve starts firing randomly. Sometimes, it’s caused by multiple sclerosis or a tumor. But in most cases, doctors can’t find a clear reason-just a nerve that’s gone rogue.
How it compares to other painful nerves
You might have heard about sciatica, phantom limb pain, or postherpetic neuralgia after shingles. All of these are incredibly painful. But none match the intensity and unpredictability of trigeminal neuralgia.
Sciatica radiates down the leg. It’s constant, burning, and frustrating-but it doesn’t strike like lightning. Phantom limb pain can feel like your missing hand is being crushed. Still, it’s usually more of a dull ache than a stabbing shock. Postherpetic neuralgia lingers for months after a rash clears, but it doesn’t come and go with the flick of a switch.
Trigeminal neuralgia is different. It’s not just pain. It’s pain that hijacks your life. A 2023 study in the Journal of Neurology found that patients with this condition reported lower quality of life than those with advanced cancer or heart failure. That’s not hyperbole. It’s data.
Treatment options-what actually works
Medications are the first line of defense. Carbamazepine, oxcarbazepine, and gabapentin are the most common. They don’t cure the nerve damage-they just try to calm the electrical chaos. About 70% of people get some relief at first. But over time, the drugs lose their power. Side effects like dizziness, fatigue, and memory fog pile up. Many patients stop taking them because the cost to their daily life becomes too high.
Surgery is the next step. The most effective procedure is microvascular decompression. Surgeons make a small opening behind the ear, move the offending blood vessel away from the nerve, and insert a tiny pad to keep it from pressing again. Success rates are around 85% in the first year. But it’s not risk-free. There’s a 1 in 50 chance of hearing loss, facial weakness, or stroke.
Other options include radiofrequency ablation, gamma knife radiation, and nerve blocks. These are less invasive but often provide only temporary relief. Some people get months of comfort. Others go back to pain within weeks.
There’s no magic bullet. Treatment is about managing, not curing. Many patients cycle through drugs, try surgery, then return to meds when the pain comes back. It’s a constant negotiation between pain and side effects, between hope and reality.

The emotional toll
Physical pain is one thing. But the isolation is worse. Because the pain is invisible, many people don’t believe it’s real. A 2024 survey in New Zealand found that 62% of trigeminal neuralgia patients had been told they were “just stressed” or “overreacting.” Some lost jobs. Others lost friends. One man from Wellington stopped attending his daughter’s school plays because he couldn’t risk a facial twitch triggering an attack.
Depression and anxiety are common. Sleep is nearly impossible when you’re afraid to fall asleep-because a dream, a turn of the head, or even your own heartbeat might set off a flare-up. Many patients carry a stress ball or a cold pack in their pocket, just in case.
What’s on the horizon
Research is moving slowly, but there’s progress. New drugs are being tested that target specific ion channels on nerve cells. One experimental treatment uses focused ultrasound to heat and disable the damaged part of the nerve without cutting into the skull. Early results are promising.
Also, neurostimulation devices are getting smaller and smarter. Some are now implanted just under the skin near the jaw, sending gentle pulses to block pain signals. They’re not perfect-they can malfunction, need battery replacements, or cause tingling-but for some, they’ve been life-changing.
What’s clear is that this isn’t just a medical issue. It’s a human one. People with trigeminal neuralgia aren’t just managing pain. They’re rebuilding their lives, one quiet moment at a time.
Can trigeminal neuralgia go away on its own?
In rare cases, yes. A small number of people experience one or two episodes and never have another. But for most, the condition is chronic and tends to worsen over time. Episodes become more frequent and last longer. Waiting for it to disappear isn’t a reliable strategy-early treatment is key.
Is trigeminal neuralgia the same as a migraine?
No. Migraines are throbbing headaches, often with nausea, light sensitivity, and aura. Trigeminal neuralgia is sharp, electric, and localized to the face. While some migraine sufferers report facial pain, true trigeminal neuralgia doesn’t involve head pressure or vomiting. The triggers and treatments are completely different.
Can dental work cause trigeminal neuralgia?
It can trigger it in people who already have a vulnerable nerve. A root canal, tooth extraction, or even a deep filling might set off the first attack. But dental procedures don’t cause the underlying nerve damage. That’s usually due to blood vessel pressure or nerve degeneration. Still, if pain starts after dental work, it’s worth getting checked by a neurologist.
Why is it called the ‘suicide disease’?
It’s a grim nickname used by some patients and doctors because the pain is so unbearable that some have considered ending their lives. This term is outdated and stigmatizing, but it reflects how extreme the suffering can be. Today, the focus is on better treatments and reducing stigma-not labeling it.
Are there any lifestyle changes that help?
Yes. Avoiding cold drafts, eating soft foods, and using a straw can reduce triggers. Some find relief with gentle facial massage or applying warm compresses. Stress management matters too-high stress levels can make attacks more frequent. Meditation, breathing exercises, and therapy can help, even if they don’t stop the pain entirely.